Blast exposure is changing how the brain–gut axis is understood in military and first responder medicine, and those insights matter directly for how Mind Spa Denver thinks about Veteran and tactical mental health care. Emerging research now shows that repeated low-level blast does not just affect the brain; it measurably alters gut permeability and is linked to concussion-like cognitive symptoms, opening up new targets for prevention and treatment.
Recent work in Military Medicine and related journals has tracked what happens to service members during realistic training with mortars and breaching charges. In these studies, soldiers exposed to low-level blast overpressure showed:
In mortarmen, greater blast intensity was associated with larger changes in gut permeability markers, and shifts in LBP and Claudin‑3 tracked with the severity of cognitive and concussion-like symptoms. These converging data strongly support a link between blast exposure, gut barrier disruption, and brain-related complaints, reinforcing the concept that the gut–brain axis is a key part of blast injury biology.
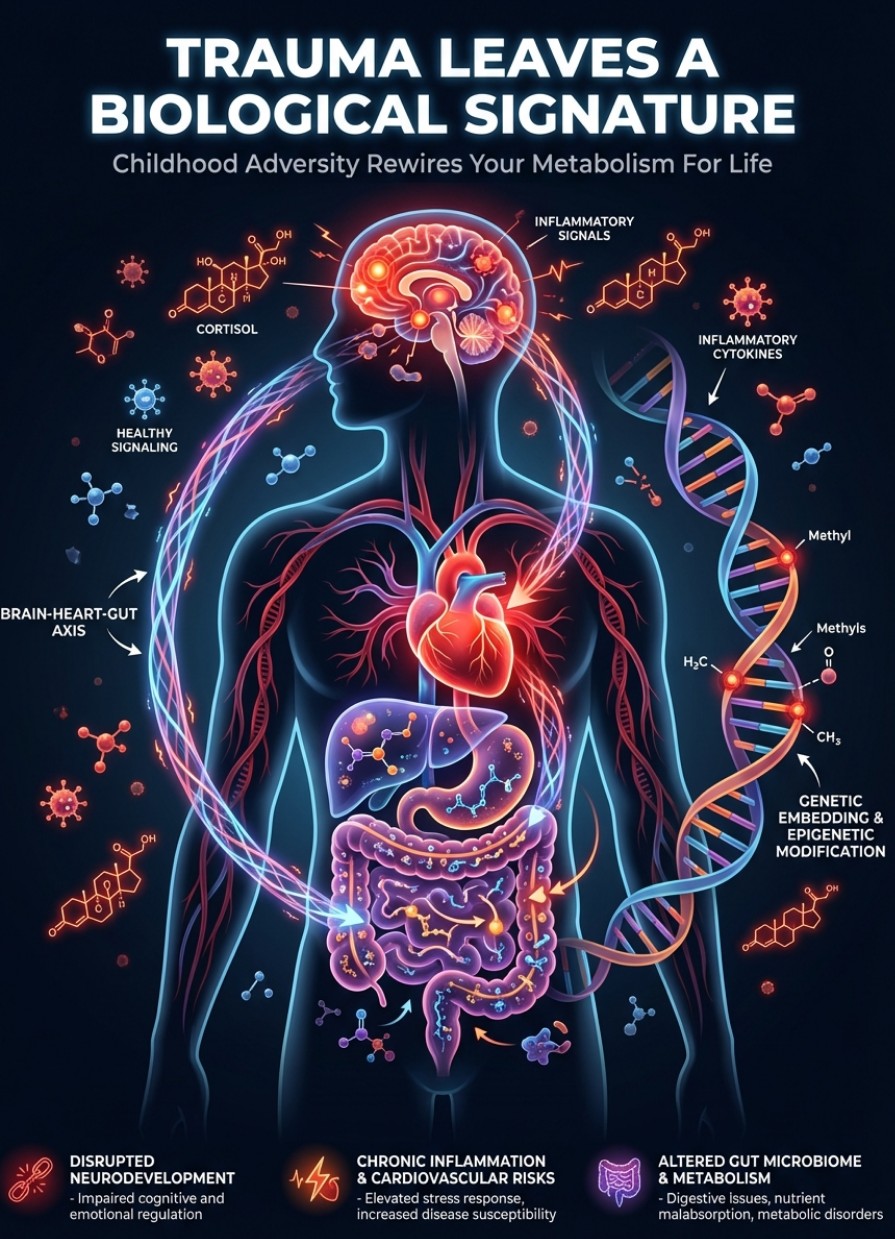
For mortarmen, EOD technicians, breachers, artillery crews, and other tactical professionals, low-level blast is not a rare event; it is built into the job. Historically, many of these exposures were considered “safe” if they stayed under certain pressure thresholds or did not produce obvious concussions, but current research is challenging that assumption. When intestinal permeability increases, inflammatory and immune signals can rise systemically and may add to the burden on the brain, especially in those with prior mild traumatic brain injury. Over time, this repeated insult could help explain why some Veterans and first responders experience a mix of:
These findings align with a broader shift in the field away from viewing “invisible wounds” as purely psychological and toward understanding them as integrated brain–body conditions that involve the gut, immune system, and nervous system together.
Mind Spa Denver specializes in interventional psychiatry and layered, whole-person care for depression, PTSD, and complex trauma, including in Veteran and first responder populations. The emerging blast–gut–brain data reinforce several principles already at the core of Mind Spa’s model:
As research continues to clarify how blast exposure drives changes in gut permeability and inflammation, targeting the gut–brain axis may become an increasingly important part of caring for those with operational blast histories. Clinics like Mind Spa are uniquely positioned to adapt as new biomarkers and treatment strategies emerge because the care model already prioritizes individualized, multi-modal plans over one-size-fits-all protocols.
The latest blast and gut-permeability studies suggest that monitoring intestinal biomarkers could one day help identify service members and Veterans at higher risk for persistent cognitive and mood symptoms after repeated blast exposure. While this is not yet standard clinical practice, it underscores the importance of collaborative care models where psychiatry, primary care, and, eventually, gastroenterology and immunology can work together for high-risk groups.
Mind Spa Denver will continue to track developments in blast and gut–brain research while providing Veteran- and responder-informed care with advanced treatments like TMS, ketamine therapy, mHBOT, and trauma-focused psychotherapy. For those who have lived their careers on the blast line, the message from the science is validating: the symptoms are real, they have a biological footprint, and there are evolving ways to approach healing that honor the full complexity of the injury.