People who live with treatment-resistant depression, PTSD, anxiety, or persistent post-concussive symptoms often describe the same frustrating pattern: they can understand what is happening intellectually, but their brain and body do not reliably follow.
Inner Armor is built around a straightforward clinical idea supported by modern neuroscience: complex syndromes are rarely driven by a single bottleneck. They often involve a combination of impaired network regulation (especially prefrontal control), disrupted neuroplasticity, and physiologic stressors that can amplify symptoms, including sleep disruption and inflammatory signaling. Psychiatry Online+2PMC+2
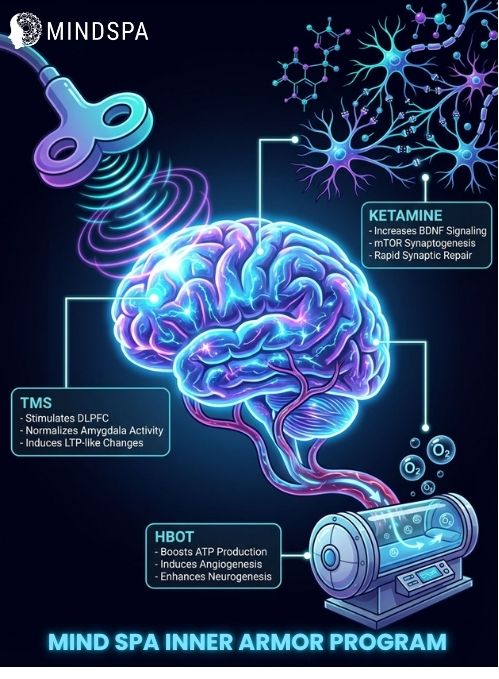
That is why Inner Armor stacks three neuromodulatory interventions, transcranial magnetic stimulation (TMS), ketamine infusions, and hyperbaric oxygen therapy (HBOT), alongside trauma-informed psychotherapy. Each modality targets a different aspect of neurobiology. The intended convergence is the same: healthier circuit connectivity, improved capacity for learning and updating, and stronger prefrontal “top-down” regulation.
Important note: the strongest clinical evidence base is for each modality individually in its best-supported indications. Evidence for combining modalities is emerging and is not yet definitive, especially for triple-modality protocols. PMC+1
Most FDA-cleared depression TMS protocols target the dorsolateral prefrontal cortex (DLPFC), typically with high-frequency stimulation over the left DLPFC. Large multisite sham-controlled trials support antidepressant efficacy, and meta-analyses of randomized trials show clinically meaningful response and remission benefits versus sham. JAMA Network+2Cambridge University Press & Assessment+2
Real-world outcomes vary by population, protocol, and measurement, but contemporary reviews commonly report remission rates in the range of roughly 25 to 30% in clinical practice, with some registries reporting higher values in specific settings. PMC+1
Why the DLPFC matters clinically: convergent neuroimaging literature in PTSD and depression supports the model of altered prefrontal regulation of threat and emotion networks, including limbic regions such as the amygdala. JAMA Network+2Nature+2
Ketamine is best-known clinically for its rapid antidepressant effects in treatment-resistant depression, often observed within hours to days in controlled studies and clinical practice. Nature+1
Mechanistically, leading models describe NMDA receptor antagonism that increases glutamatergic throughput and downstream AMPA signaling, with involvement of plasticity-related pathways including BDNF and mTOR in preclinical and translational work. PMC+2Nature+2
Ketamine is also being actively studied for immunomodulatory and anti-inflammatory effects, with reviews describing cytokine-related changes across preclinical and clinical contexts, although human findings remain heterogeneous and should not be oversold. PMC+1
HBOT increases the amount of dissolved oxygen in plasma under elevated pressure, which can increase oxygen delivery to tissues beyond what hemoglobin transport alone provides. Taylor & Francis Online+1
In persistent post-concussion symptom populations, several clinical studies report cognitive and symptom improvements, and advanced imaging studies describe changes consistent with neuroplasticity, including perfusion and microstructural metrics. PLOS+2PMC+2
At the same time, HBOT in TBI-related syndromes has been an area of debate, with variability across trial designs (including sham conditions), protocols, and endpoints. Systematic reviews emphasize the importance of dose, pressure, and careful interpretation. PubMed+1
HBOT is also being studied for effects on neuroinflammatory pathways in TBI models and broader inflammatory contexts, including evidence of reduced neuroinflammatory markers in preclinical work and cytokine shifts reported in systematic reviews. PMC+1
Emerging clinical research has also examined HBOT in combat-associated PTSD with randomized sham-controlled designs, reporting symptom and connectivity changes, though replication and broader validation remain important. PubMed+1
Depression and PTSD have substantial literature linking subsets of patients to inflammatory and immune dysregulation signals, including meta-analytic evidence in PTSD and mechanistic reviews in depression and microglia-related pathways. ScienceDirect+2PMC+2
Inner Armor’s rationale is not that “inflammation causes everything,” but that inflammatory signaling can be a meaningful modifier of symptom severity, recovery capacity, and neuroplasticity in some patients. Cell+1
rTMS has evidence consistent with inducing durable neuroplastic changes, often framed as LTP-like mechanisms and measurable functional connectivity shifts across studies and reviews. Psychiatry Online+2ScienceDirect+2
Ketamine adds a different plasticity profile, with rapid synaptic and circuit effects supported by translational neuroscience literature. Nature+1
HBOT is studied as a biologic intervention that can influence perfusion, angiogenesis-related signals, and imaging markers associated with cognitive improvement in some chronic post-concussion and TBI-related samples. PMC+2PLOS+2
The goal of trauma-informed psychotherapy within a neuromodulation-forward program is practical: translate improved plasticity and regulation capacity into durable skills, updated threat learning, and healthier patterns of attention and interpretation. Evidence syntheses in PTSD support the centrality of prefrontal systems in threat regulation and recovery. Nature+1
Standard antidepressants often require weeks for full clinical effect, and large effectiveness studies illustrate that remission at the first medication step is commonly in the range of about 28 to 33% depending on measurement, with decreasing remission rates across subsequent steps in more treatment-resistant trajectories. PubMed+1
Inner Armor is designed around a constrained systems view:
What the evidence currently supports: combining TMS and ketamine has early literature, including reviews that primarily include case reports, retrospective cohorts, and small clinical samples. This is promising but not yet the same as high-quality, large randomized trials of combination therapy. PMC+2Brain Stimulation Journal+2
Inner Armor is typically most relevant for individuals with:
Appropriateness depends on diagnosis, medical history, medications, and safety screening. Ketamine and HBOT, in particular, require careful medical evaluation and protocol selection.
Does TMS “activate” the prefrontal cortex?
TMS can modulate cortical excitability and network activity. Clinical trials support antidepressant efficacy when applied to prefrontal targets, and reviews describe plasticity-consistent mechanisms. JAMA Network+2Psychiatry Online+2
How fast does ketamine work for depression?
In treatment-resistant depression research and clinical settings, ketamine can produce antidepressant effects within hours to days, though durability varies and typically requires an ongoing treatment plan. Nature+1
Is HBOT proven for chronic TBI or PTSD?
The literature includes positive studies and ongoing debate. Some trials and imaging studies report improvements in persistent post-concussion symptoms and related cognitive measures, and there are sham-controlled PTSD studies in veterans. Interpretation requires attention to protocols, endpoints, and replication. hsrd.research.va.gov+3PubMed+3PLOS+3
Is there strong evidence that combining TMS, ketamine, and HBOT is better than each alone?
Not yet at a high-confidence level. Evidence for combining TMS and ketamine is emerging but is largely based on smaller studies. Evidence for triple-modality stacking is currently more rationale-driven than trial-proven. PMC+1